Cardiac Output
Cardiac output (Q or Qc ) is the volume of blood being pumped by the heart, in particular by a left or right ventricle in the time interval of one minute. CO may be measured in many ways, for example dm3/min (1 dm3 equals 1000 cm3 or 1 litre). Q is furthermore the combined sum of output from the right ventricle and the output from the left ventricle during the phase of systole of the heart. An average resting cardiac output would be 5.6 L/min for a human male and 4.9 L/min for a female.
Q=Stroke Volume × Heart rate
Heart is a 'demand pump', that pumps out whatever blood comes back into it from the venous system, it is effectively the amount of blood returning to the heart that determines how much blood the heart pumps out (Q).
Stroke Volume (SV) = EDV – ESV
Ejection Fraction (EF) = (SV / EDV) × 100%
Cardiac Output (Q) = SV × HR
Measuring cardiac output
The Fick PrincipleThe Fick principle was first described by Adolf Eugen Fick in 1870 and assumes that the rate at which oxygen is consumed is a function of the rate of blood flows and the rate of oxygen picked up by the red blood cells. The Fick principle involves calculating the oxygen consumed over a given period of time from measurement of the oxygen concentration of the venous blood and the arterial blood. Q can be calculated from these measurements:
- VO2 consumption per minute using a spirometer (with the subject re-breathing air) and a CO2 absorber
- the oxygen content of blood taken from the pulmonary artery (representing mixed venous blood)
- the oxygen content of blood from a cannula in a peripheral artery (representing arterial blood)
From these values, we know that:
VO2 = (Q×CA) - (Q×CV)
where
- CA = Oxygen content of arterial blood
- CV = Oxygen content of venous blood.
This allows us to say
Q = (VO2/[CA - CV])*100
and therefore calculate Q.Dilution methods
Impedance cardiography
Impedance cardiography (often related as ICG or TEB) is a method that measures changes in impedance across the thoracic region over the cardiac cycle. Lower impedance indicates greater the intrathoracic fluid volume and blood flow. Therefore, by synchronizing fluid volume changes with heartbeat, the change in impedance can be used to calculate stroke volume, cardiac output, and systemic vascular resistance. Both invasive and non-invasive approaches are being used.
The noninvasive approach has achieved some acceptance with respect to its reliability and validity. The clinical use of this approach in a variety of diseases continues.
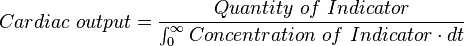
This method was initially described using an indicator dye and assumes that the rate at which the indicator is diluted reflects the Q. The method measures the concentration of a dye at different points in the circulation, usually from an intravenous injection and then at a downstream sampling site, usually in a systemic artery. More specifically, the Q is equal to the quantity of indicator dye injected divided by the area under the dilution curve measured downstream (the Stewart (1897)-Hamilton (1932) equation):
The trapezoid rule is often used as an approximation of this integral.
Pulmonary Artery Thermodilution (Trans-right-heart Thermodilution)
The indicator method was further developed with replacement of the indicator dye by heated or cooled fluid and temperature change measured at different sites in the circulation rather than dye concentration; this method is known as thermodilution. The pulmonary artery catheter (PAC), also known as the Swan-Ganz catheter, was introduced to clinical practice in 1970 and provides direct access to the right heart for thermodilution measurements.
The PAC is balloon tipped and is inflated, which helps "sail" the catheter balloon through the right ventricle to occlude a smaller branch of the pulmonary artery system. The balloon is deflated. The PAC thermodilution method involves injection of a small amount (10ml) of cold glucose at a known temperature into the pulmonary artery and measuring the temperature a known distance away (6–10 cm) using the same catheter.
The Q can be calculated from the measured temperature curve (The “thermodilution curve”). High Q will change the temperature rapidly, and low Q will change the temperature slowly. Usually three or four repeated measures are averaged to improve accuracy.Impedance cardiography
Impedance cardiography (often related as ICG or TEB) is a method that measures changes in impedance across the thoracic region over the cardiac cycle. Lower impedance indicates greater the intrathoracic fluid volume and blood flow. Therefore, by synchronizing fluid volume changes with heartbeat, the change in impedance can be used to calculate stroke volume, cardiac output, and systemic vascular resistance. Both invasive and non-invasive approaches are being used.
The noninvasive approach has achieved some acceptance with respect to its reliability and validity. The clinical use of this approach in a variety of diseases continues.

No comments:
Post a Comment