Introduction to Biomedical Engineering
Who is a Biomedical Engineer?
A Biomedical Engineer uses traditional engineering expertise to analyze and solve problems
in biology and medicine, providing an overall enhancement of health care. Students choose
the biomedical engineering field to be of service to people, to partake of the excitement of
working with living systems, and to apply advanced technology to the complex problems of
medical care. The biomedical engineer works with other health care professionals including
physicians, nurses, therapists and technicians. Biomedical engineers may be called upon in
a wide range of capacities: to design instruments, devices, and software, to bring together
knowledge from many technical sources to develop new procedures, or to conduct research
needed to solve clinical problems.
What are Some of the Specialty Areas?
In this field there is continual change and creation of new areas due to rapid advancement
in technology; however, some of the well established specialty areas within the field of
biomedical engineering are: bioinstrumentation; biomaterials; biomechanics; cellular,
tissue and genetic engineering; clinical engineering; medical imaging; orthopaedic surgery;
rehabilitation engineering; and systems physiology.
Bioinstrumentation is the application of electronics and measurement techniques to
develop devices used in diagnosis and treatment of disease. Computers are an essential
part of bioinstrumentation, from the microprocessor in a single-purpose instrument used to
do a variety of small tasks to the microcomputer needed to process the large amount of
information in a medical imaging system.
Biomaterials include both living tissue and artificial materials used for implantation.
Understanding the properties and behavior of living material is vital in the design of
implant materials. The selection of an appropriate material to place in the human body
may be one of the most difficult tasks faced by the biomedical engineer. Certain metal
alloys, ceramics, polymers, and composites have been used as implantable materials.
Biomaterials must be nontoxic, non-carcinogenic, chemically inert, stable, and
mechanically strong enough to withstand the repeated forces of a lifetime. Newer
biomaterials even incorporate living cells in order to provide a true biological and
mechanical match for the living tissue.
Biomechanics applies classical mechanics (statics, dynamics, fluids, solids,
thermodynamics, and continuum mechanics) to biological or medical problems. It includes
the study of motion, material deformation, flow within the body and in devices, and
transport of chemical constituents across biological and synthetic media and membranes.
Progress in biomechanics has led to the development of the artificial heart and heart
valves, artificial joint replacements, as well as a better understanding of the function of the
heart and lung, blood vessels and capillaries, and bone, cartilage, intervertebral discs,
ligaments and tendons of the musculoskeletal systems.
Cellular, Tissue and Genetic Engineering involve more recent attempts to attack
biomedical problems at the microscopic level. These areas utilize the anatomy,
biochemistry and mechanics of cellular and sub-cellular structures in order to understand
disease processes and to be able to intervene at very specific sites. With these capabilities,
miniature devices deliver compounds that can stimulate or inhibit cellular processes at
precise target locations to promote healing or inhibit disease formation and progression.
Clinical Engineering is the application of technology to health care in hospitals. The
clinical engineer is a member of the health care team along with physicians, nurses and
other hospital staff. Clinical engineers are responsible for developing and maintaining
computer databases of medical instrumentation and equipment records and for the
purchase and use of sophisticated medical instruments. They may also work with
physicians to adapt instrumentation to the specific needs of the physician and the hospital.
This often involves the interface of instruments with computer systems and customized
software for instrument control and data acquisition and analysis. Clinical engineers are
involved with the application of the latest technology to health care.
Medical Imaging combines knowledge of a unique physical phenomenon (sound,
radiation, magnetism, etc.) with high speed electronic data processing, analysis and
display to generate an image. Often, these images can be obtained with minimal or
completely noninvasive procedures, making them less painful and more readily repeatable
than invasive techniques.
Orthopaedic Bioengineering is the specialty where methods of engineering and
computational mechanics have been applied for the understanding of the function of bones,
joints and muscles, and for the design of artificial joint replacements. Orthopaedic
bioengineers analyze the friction, lubrication and wear characteristics of natural and
artificial joints; they perform stress analysis of the musculoskeletal system; and they
develop artificial biomaterials (biologic and synthetic) for replacement of bones, cartilages,
ligaments, tendons, meniscus and intervertebral discs. They often perform gait and motion
analyses for sports performance and patient outcome following surgical procedures.
Orthopaedic bioengineers also pursue fundamental studies on cellular function, and
mechano-signal transduction.
Rehabilitation Engineering is a growing specialty area of biomedical engineering.
Rehabilitation engineers enhance the capabilities and improve the quality of life for
individuals with physical and cognitive impairments. They are involved in prosthetics, the
development of home, workplace and transportation modifications and the design of
assistive technology that enhance seating and positioning, mobility, and communication.
Rehabilitation engineers are also developing hardware and software computer adaptations
and cognitive aids to assist people with cognitive difficulties.
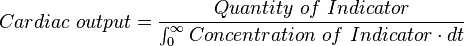
Systems Physiology is the term used to describe that aspect of biomedical engineering in
which engineering strategies, techniques and tools are used to gain a comprehensive and
integrated understanding of the function of living organisms ranging from bacteria to
humans. Computer modeling is used in the analysis of experimental data and in
formulating mathematical descriptions of physiological events. In research, predictor
models are used in designing new experiments to refine our knowledge. Living systems
have highly regulated feedback control systems that can be examined with state-of-the-art
techniques. Examples are the biochemistry of metabolism and the control of limb
movements.
These specialty areas frequently depend on each other. Often, the biomedical engineer who
works in an applied field will use knowledge gathered by biomedical engineers working in
other areas. For example, the design of an artificial hip is greatly aided by studies on
anatomy, bone biomechanics, gait analysis, and biomaterial compatibility. The forces that
are applied to the hip can be considered in the design and material selection for the
prosthesis. Similarly, the design of systems to electrically stimulate paralyzed muscle to
move in a controlled way uses knowledge of the behavior of the human musculoskeletal
system. The selection of appropriate materials used in these devices falls within the realm
of the biomaterials engineer.
Examples of Specific Activities
Work done by biomedical engineers may include a wide range of activities such as:
A Biomedical Engineer uses traditional engineering expertise to analyze and solve problems
in biology and medicine, providing an overall enhancement of health care. Students choose
the biomedical engineering field to be of service to people, to partake of the excitement of
working with living systems, and to apply advanced technology to the complex problems of
medical care. The biomedical engineer works with other health care professionals including
physicians, nurses, therapists and technicians. Biomedical engineers may be called upon in
a wide range of capacities: to design instruments, devices, and software, to bring together
knowledge from many technical sources to develop new procedures, or to conduct research
needed to solve clinical problems.
What are Some of the Specialty Areas?
In this field there is continual change and creation of new areas due to rapid advancement
in technology; however, some of the well established specialty areas within the field of
biomedical engineering are: bioinstrumentation; biomaterials; biomechanics; cellular,
tissue and genetic engineering; clinical engineering; medical imaging; orthopaedic surgery;
rehabilitation engineering; and systems physiology.
Bioinstrumentation is the application of electronics and measurement techniques to
develop devices used in diagnosis and treatment of disease. Computers are an essential
part of bioinstrumentation, from the microprocessor in a single-purpose instrument used to
do a variety of small tasks to the microcomputer needed to process the large amount of
information in a medical imaging system.
Biomaterials include both living tissue and artificial materials used for implantation.
Understanding the properties and behavior of living material is vital in the design of
implant materials. The selection of an appropriate material to place in the human body
may be one of the most difficult tasks faced by the biomedical engineer. Certain metal
alloys, ceramics, polymers, and composites have been used as implantable materials.
Biomaterials must be nontoxic, non-carcinogenic, chemically inert, stable, and
mechanically strong enough to withstand the repeated forces of a lifetime. Newer
biomaterials even incorporate living cells in order to provide a true biological and
mechanical match for the living tissue.
Biomechanics applies classical mechanics (statics, dynamics, fluids, solids,
thermodynamics, and continuum mechanics) to biological or medical problems. It includes
the study of motion, material deformation, flow within the body and in devices, and
transport of chemical constituents across biological and synthetic media and membranes.
Progress in biomechanics has led to the development of the artificial heart and heart
valves, artificial joint replacements, as well as a better understanding of the function of the
heart and lung, blood vessels and capillaries, and bone, cartilage, intervertebral discs,
ligaments and tendons of the musculoskeletal systems.
Cellular, Tissue and Genetic Engineering involve more recent attempts to attack
biomedical problems at the microscopic level. These areas utilize the anatomy,
biochemistry and mechanics of cellular and sub-cellular structures in order to understand
disease processes and to be able to intervene at very specific sites. With these capabilities,
miniature devices deliver compounds that can stimulate or inhibit cellular processes at
precise target locations to promote healing or inhibit disease formation and progression.
Clinical Engineering is the application of technology to health care in hospitals. The
clinical engineer is a member of the health care team along with physicians, nurses and
other hospital staff. Clinical engineers are responsible for developing and maintaining
computer databases of medical instrumentation and equipment records and for the
purchase and use of sophisticated medical instruments. They may also work with
physicians to adapt instrumentation to the specific needs of the physician and the hospital.
This often involves the interface of instruments with computer systems and customized
software for instrument control and data acquisition and analysis. Clinical engineers are
involved with the application of the latest technology to health care.
Medical Imaging combines knowledge of a unique physical phenomenon (sound,
radiation, magnetism, etc.) with high speed electronic data processing, analysis and
display to generate an image. Often, these images can be obtained with minimal or
completely noninvasive procedures, making them less painful and more readily repeatable
than invasive techniques.
Orthopaedic Bioengineering is the specialty where methods of engineering and
computational mechanics have been applied for the understanding of the function of bones,
joints and muscles, and for the design of artificial joint replacements. Orthopaedic
bioengineers analyze the friction, lubrication and wear characteristics of natural and
artificial joints; they perform stress analysis of the musculoskeletal system; and they
develop artificial biomaterials (biologic and synthetic) for replacement of bones, cartilages,
ligaments, tendons, meniscus and intervertebral discs. They often perform gait and motion
analyses for sports performance and patient outcome following surgical procedures.
Orthopaedic bioengineers also pursue fundamental studies on cellular function, and
mechano-signal transduction.
Rehabilitation Engineering is a growing specialty area of biomedical engineering.
Rehabilitation engineers enhance the capabilities and improve the quality of life for
individuals with physical and cognitive impairments. They are involved in prosthetics, the
development of home, workplace and transportation modifications and the design of
assistive technology that enhance seating and positioning, mobility, and communication.
Rehabilitation engineers are also developing hardware and software computer adaptations
and cognitive aids to assist people with cognitive difficulties.
Systems Physiology is the term used to describe that aspect of biomedical engineering in
which engineering strategies, techniques and tools are used to gain a comprehensive and
integrated understanding of the function of living organisms ranging from bacteria to
humans. Computer modeling is used in the analysis of experimental data and in
formulating mathematical descriptions of physiological events. In research, predictor
models are used in designing new experiments to refine our knowledge. Living systems
have highly regulated feedback control systems that can be examined with state-of-the-art
techniques. Examples are the biochemistry of metabolism and the control of limb
movements.
These specialty areas frequently depend on each other. Often, the biomedical engineer who
works in an applied field will use knowledge gathered by biomedical engineers working in
other areas. For example, the design of an artificial hip is greatly aided by studies on
anatomy, bone biomechanics, gait analysis, and biomaterial compatibility. The forces that
are applied to the hip can be considered in the design and material selection for the
prosthesis. Similarly, the design of systems to electrically stimulate paralyzed muscle to
move in a controlled way uses knowledge of the behavior of the human musculoskeletal
system. The selection of appropriate materials used in these devices falls within the realm
of the biomaterials engineer.
Examples of Specific Activities
Work done by biomedical engineers may include a wide range of activities such as:
- Artificial organs (hearing aids, cardiac pacemakers, artificial kidneys and hearts, blood oxygenators, synthetic blood vessels, joints, arms, and legs).
- Automated patient monitoring (during surgery or in intensive care, healthy persons in unusual environments, such as astronauts in space or underwater divers at great depth).
- Blood chemistry sensors (potassium, sodium, O2, CO2, and pH).
- Advanced therapeutic and surgical devices (laser system for eye surgery, automated delivery of insulin, etc.).
- Application of expert systems and artificial intelligence to clinical decision making (computer-based systems for diagnosing diseases).
- Design of optimal clinical laboratories (computerized analyzer for blood samples, cardiac catheterization laboratory, etc.).
- Medical imaging systems (ultrasound, computer assisted tomography, magnetic resonance imaging, positron emission tomography, etc.).
- Computer modeling of physiologic systems (blood pressure control, renal function, visual and auditory nervous circuits, etc.).
- Biomaterials design (mechanical, transport and biocompatibility properties of implantable artificial materials).
- Biomechanics of injury and wound healing (gait analysis, application of growth factors, etc.).
- Sports medicine (rehabilitation, external support devices, etc.).